
You will find on this page
What is Gestational Diabetes?
How does gestational diabetes develop?
Who Is at Higher Risk?
Symptoms of Gestational Diabetes
How Is Gestational Diabetes Diagnosed?
Does Gestational Diabetes Affect the Baby?
What is Gestational Diabetes?
Gestational diabetes is a type of diabetes that is first diagnosed during pregnancy, typically between weeks 24 and 28. It occurs when blood sugar levels rise due to the body's inability to produce enough insulin to meet the demands of pregnancy. This happens because hormonal changes affect the body's response to insulin, leading to elevated blood sugar levels.
Who Is at Higher Risk?
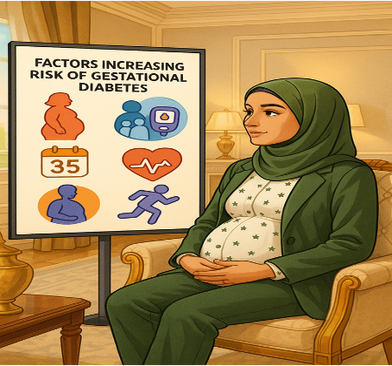
Several factors increase the risk of developing gestational diabetes, including:
- Obesity or being overweight before pregnancy
- A family history of diabetes
- Having had gestational diabetes in a previous pregnancy
- Advanced maternal age (over 35 years old)
- High blood pressure or cardiovascular disease
- Lack of physical activity before and during pregnancy
Symptoms of Gestational Diabetes

Gestational diabetes is typically detected through routine prenatal screenings at 24-28 weeks and most women do not experience any symptoms
However, in some cases, the following symptoms may occur:
- Increased thirst
- frequent urination
- Fatigue
- Blurred vision
How Is Gestational Diabetes Diagnosed?
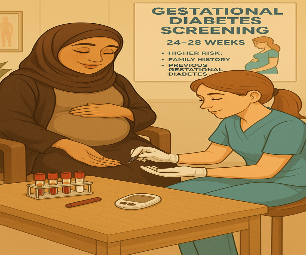
Gestational diabetes is usually diagnosed between 24 and 28 weeks of pregnancy through routine blood glucose testing. Women at higher risk, such as those with a history of gestational diabetes or a family history of diabetes, may be tested earlier. Knowing your diagnosis early helps you take steps to manage your health and protect your baby.
How Gestational Diabetes Affect my baby’s health when I have gestational diabetes?

The Gestational Diabetes will affect your lifestyle to be healthier and active. If you keep your sugar level stable and in normal range, there will be minimum effect on your baby’s health or your own health. But sometimes regardless of what you do, the pregnancy hormones can change the level of your blood sugar. The your blood sugar keep going higher, then you may have a risk of :
- Increased Birth Weight (Macrosomia):
- Elevated maternal glucose levels result in increased glucose transfer to the fetus, stimulating fetal insulin production and leading to excessive fat accumulation and growth. This increases the risk of difficult deliveries and birth injuries.
- Preterm Birth:
- GDM may raise the risk of early labor, exposing the baby to health issues associated with prematurity.
- Neonatal Hypoglycemia:
- Post-delivery, the baby may continue to produce high insulin levels, leading to low blood sugar levels.
- Respiratory Distress:
- Babies born to mothers with GDM might experience breathing difficulties due to delayed lung maturation.
- Increased Risk of Obesity and Type 2 Diabetes Later in Life
✨ Did you know long-term Breastfeeding can protect you and your baby from getting diabetes later on in your life?
Your pregnancy journey is beautiful, and your health and your baby’s well-being are in your hands! ✨Managing your blood sugar levels is the key to a healthy pregnancy and a safe delivery. With regular check-ups, balanced nutrition, moderate physical activity, and planning to breastfeed your baby, you can reduce risks and give your baby the best start in life, while also protecting your own health in the long term.

Believe in yourself—you are stronger than you think! 💪😊
💡 Being diagnosed with gestational diabetes may feel overwhelming, but don't worry! 💡
You can manage your blood sugar levels and have a healthy pregnancy for both you and your baby. There are effective diet controlled or treatment options and plenty of support available to guide you on this journey. ✨
What to do when you have been diagnosed with gestational diabetes:
Most women are diagnosed with gestational diabetes between 24–28 weeks of pregnancy.
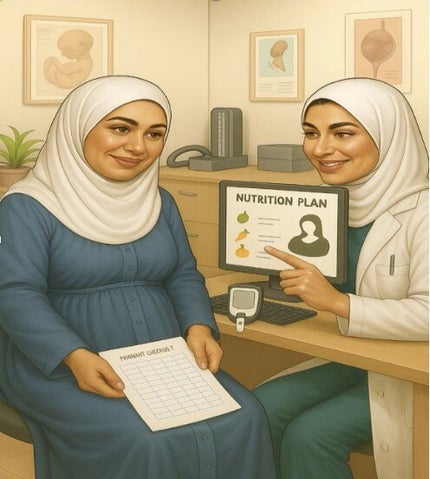
After diagnosis:
-
You will usually be reviewed in the antenatal clinic.
-
You may meet with the diabetes nurse, dietician, and/or endocrinologist.
-
You will continue antenatal visits with your midwife or obstetrician.
-
This is a good time to start planning for breastfeeding and to discuss your plan with your healthcare team.
Create Your Own Website With Webador